Balkhy, H. H., Grossi, E. A., Kiaii, B., Murphy, D., Geirsson, A., Guy, S., & Lewis, C. (2023). A Retrospective Evaluation of Endo-Aortic Balloon Occlusion Compared to External Clamping in Minimally Invasive Mitral Valve Surgery. Seminars in thoracic and cardiovascular surgery, S1043-0679(23)00040-0. Advance online publication. https://doi.org/10.1053/j.semtcvs.2022.11.016
Abstract
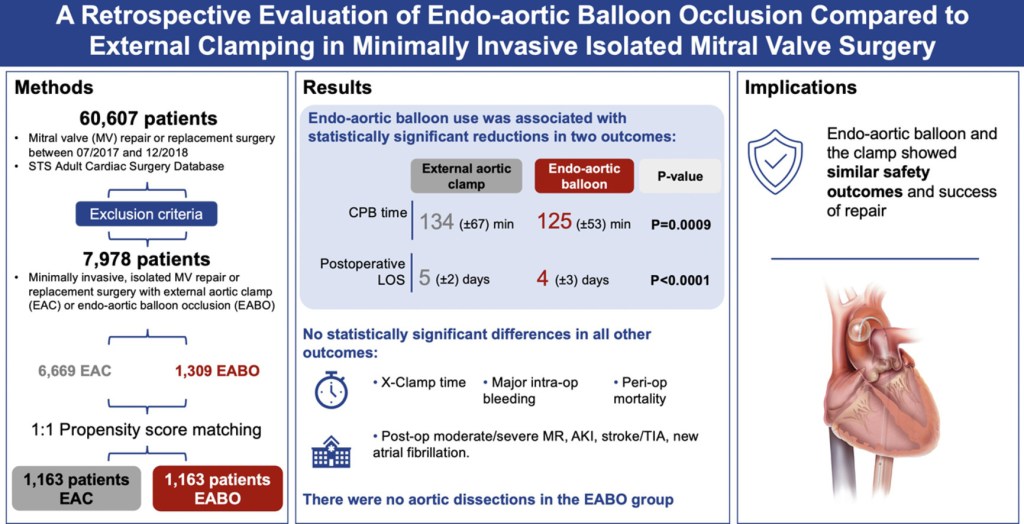
We compare outcomes of endo-aortic balloon occlusion (EABO) vs external aortic clamping (EAC) in patients undergoing minimally invasive mitral valve surgery (MIMVS) in the Society of Thoracic Surgeons (STS) Adult Cardiac Surgery Database. Adults undergoing mitral valve surgery (July 2017–December 2018) were identified within the STS database (N = 60,607). Total 7,978 patients underwent a minimally invasive approach (including robotically assisted). About 1,163 EABO patients were 1:1 propensity-matched to EAC patients using exact matching on age, sex, and type of mitral procedure, and propensity score average matching for 16 other risk indicators. Early outcomes were compared. Categorical variables were compared using logistic regression; hospital and intensive care unit length of stay were compared using negative binomial regression. In the matched cohort, mean age was 62 years; 35.9% were female, and 86% underwent mitral valve repair. Cardiopulmonary bypass time was shorter for EABO vs EAC group (125.0 ± 53.0 vs 134.0 ± 67.0 minutes, P = 0.0009). There was one aortic dissection in the EAC group and none in the EABO group (P value > 0.31), and no statistically significant differences in cross-clamp time, major intraoperative bleeding, perioperative mortality, stroke, new onset of atrial fibrillation, postoperative acute kidney injury, success of repair. Median hospital LOS was shorter for EABO vs EAC procedures (4 vs 5 days, P < 0.0001). In this large, retrospective, STS database propensity-matched analysis ofpatients undergoing MIMVS, we observed similar safety outcomes for EABO and EAC, including no aortic dissections in the EABO group. The EABO group showed slightly shorter CPB times and hospital LOS.
Graphical Abstract